Do Probiotics for Celiac Disease Contain Gluten? The Evidence-Based Ultimate Guide
Can celiac-safe probiotics contain gluten? Learn how to verify labels, spot hidden gluten risks, compare evidence, and choose lower-risk supplements confidently.
11 Min Read
Do Probiotics for Celiac Disease Contain Gluten? The Evidence-Based Ultimate Guide
If you have celiac disease, you already know the daily math: every label matters, every ingredient list matters, and every supplement decision can feel like a risk calculation. Probiotics are often marketed as gut-supportive, but many people with celiac disease ask a more urgent question first: can this product expose me to gluten?
The short answer is that some probiotics can carry gluten risk, but many do not. The longer and more useful answer is that risk depends on manufacturing controls, ingredient sourcing, labeling quality, and your own total daily exposure. A "gluten-free" claim helps, but it is not the only signal you should use. For celiac disease, the goal is not perfect certainty in a messy marketplace. The goal is lowering risk consistently with a repeatable process.
This guide walks through what current evidence says about contamination risk, how U.S. labeling rules actually work for dietary supplements, what clinical trials show about probiotics in celiac disease, and when probiotics are reasonable to test versus when they are a distraction from core disease management. If you want broader background before diving in, these related explainers can help with fundamentals: health benefits of probiotic foods and supplements, probiotic strains and species research, and how to know probiotic supplements are working.
Quick clinical takeaway: Probiotics are not a replacement for a strict gluten-free diet in celiac disease. Think of them as optional adjuncts only after label safety and diagnosis-guided follow-up are in place.
Can a probiotic labeled "gluten-free" still expose you to gluten?
It can, in theory, but your real-world risk depends on dose, frequency, and product quality controls. In the United States, the FDA standard for a "gluten-free" claim is less than 20 parts per million (ppm), and that framework applies to foods and dietary supplements under FDA labeling rules. That threshold is useful because it creates a measurable target, but it does not mean every product on every shelf is equally reliable in day-to-day manufacturing practice.
Why the uncertainty? Supplements are regulated differently from prescription drugs. Manufacturers are responsible for safety and labeling compliance, and FDA enforcement generally happens through oversight and post-market action rather than premarket approval of each product. That model works best when companies use strong quality systems and third-party verification, and less well when quality controls are weak.
For people with celiac disease, this means a practical mindset is essential. Instead of asking only, "Does the front label say gluten-free?" ask, "How strong is the total safety signal from this product?" A strong signal includes a clear gluten-free statement, transparent inactive ingredients, allergen disclosure, and a manufacturer that can describe contamination controls. A weak signal is vague language, proprietary blends with little detail, and no meaningful manufacturing information.
One older but still frequently discussed data point came from conference screening work presented at Digestive Disease Week in 2015, where some probiotic products marketed as gluten-free still had detectable gluten and a minority exceeded 20 ppm. Because conference abstracts are preliminary and not always peer-reviewed in full publication form, they should be interpreted cautiously. But they reinforce an important point: celiac-safe shopping requires more than blind trust in a front-panel claim.
Most celiac experts still center one treatment above all others: a strict gluten-free diet

If you read enough probiotic advertising, it can sound as if microbial supplements are the main event in gut recovery. They are not. Major clinical guidance remains clear: in confirmed celiac disease, the primary treatment is lifelong strict gluten avoidance, with follow-up to assess symptom response, nutritional status, and mucosal recovery when indicated (Rubio-Tapia et al., American Journal of Gastroenterology, 2023).
This matters because persistent symptoms are common, and the cause is not always "you need a stronger probiotic." Ongoing symptoms may reflect inadvertent gluten exposure, lactose intolerance, IBS overlap, microscopic colitis, small intestinal bacterial overgrowth, pancreatic insufficiency, thyroid disease, or, less commonly, refractory celiac disease. If probiotics are used, they should be part of a structured plan, not a substitute for proper diagnostic follow-up.
NIDDK guidance is similarly practical for daily life: check labels carefully, especially for foods, supplements, and medications, because gluten can appear in unexpected products. They also note that medications are a less common gluten source than food, but people with celiac disease should still ask when ingredient information is unclear. That logic applies to probiotics too: low-probability risks still matter when exposure is repeated every day.
If your broader symptom picture includes suspected food reactivity or confusion between gluten exposure and other triggers, this companion article can help organize pattern tracking: allergies and food sensitivities tips.
"Check the inactive ingredients first" is the advice pharmacists repeat for a reason

Many people focus on the probiotic strain name and CFU count while overlooking excipients, flavor systems, coating materials, and processing aids. For celiac disease safety, those supporting ingredients often matter more than the headline strain.
Potential gluten exposure can enter through flavor powders, malt-based ingredients, wheat-derived starches, or cross-contact in shared production lines. The exact risk of each ingredient depends on source and processing, so you should avoid overgeneralizing. For example, starches can be derived from multiple sources, and "natural flavors" can hide sourcing details that are not obvious from label language alone.
The NIH Office of Dietary Supplements also notes a quality reality that consumers should remember: the identity and number of microorganisms in a probiotic product may not always match what labels imply, and commercial formulations can vary substantially. That does not prove gluten contamination, but it is another reason to prioritize manufacturers with stronger transparency and testing culture.
| Label signal | Why it matters in celiac disease | Risk direction | Best next step |
|---|---|---|---|
| Explicit "gluten-free" claim | Suggests product is marketed to FDA threshold standards | Lower (not zero) | Confirm manufacturer testing approach if highly sensitive |
| Vague flavor blend or proprietary inactive ingredients | Harder to trace gluten sources | Higher uncertainty | Contact manufacturer or choose a clearer label |
| No allergen or cross-contact language | Missing context for contamination control | Higher uncertainty | Prefer products with explicit allergen handling disclosure |
| Third-party gluten certification | Adds an extra verification layer beyond self-claim | Lower | Use as one decision factor, not the only one |
If you are comparing strain claims at the same time, this explainer helps decode species-level language without hype: probiotic strains and species benefits research.
Why 20 ppm matters, and why dose still matters more than a label alone
The 20 ppm benchmark is a regulatory threshold, not a biological cliff where 19 ppm is always harmless and 21 ppm is always catastrophic. In celiac disease, cumulative dose over time matters. Controlled challenge data from Catassi and colleagues in the American Journal of Clinical Nutrition (2007) suggested that higher daily gluten exposure clearly worsens histology and symptoms, while lower daily amounts are generally better tolerated. Clinically, the practical principle is to keep total daily exposure as low as possible.
This is why one product may look acceptable in isolation yet still become part of a bigger problem if multiple "small" exposures stack across the day. If a person takes a probiotic, multivitamin, protein powder, flavored medication, and occasional snack products with uncertain controls, total risk increases even when each individual item seems minor.
For that reason, celiac-safe supplement strategy should be portfolio-based, not product-by-product. Minimize the number of uncertain products you use repeatedly. Choose simpler formulations. Reassess every new supplement before adding it to an already crowded routine. The strongest protection often comes from reducing complexity.
| Approach | What it looks like in real life | Expected celiac safety impact |
|---|---|---|
| Single-product thinking | "This one probiotic says gluten-free, so I am done" | Partial protection only |
| Portfolio thinking | Review all daily supplements, meds, and repeat packaged foods | Better total exposure control |
| Periodic re-audit | Re-check labels every refill or brand reformulation cycle | Prevents drift in risk over time |
What does the clinical evidence say about probiotics for celiac symptoms and inflammation?
Evidence is promising in places but still not strong enough to treat probiotics as standard celiac therapy. A 2020 systematic review in Frontiers in Nutrition found potential benefits in gastrointestinal symptom patterns and some inflammatory markers, but also substantial heterogeneity across strains, doses, duration, and trial design. A 2023 meta-analysis in Nutrients reached a similar conclusion: signal for benefit in selected outcomes, but limited certainty and inconsistent endpoints.
The central issue is not whether probiotics can influence the gut. They can. The issue is whether current probiotic evidence in diagnosed celiac disease is robust enough to change standard-of-care management. Right now, that answer is no. Guideline bodies continue to prioritize strict gluten avoidance, structured follow-up, and correction of nutritional deficiencies first.
That said, "not standard therapy" does not mean "never useful." Some patients with functional GI overlap may report symptom improvement with specific strains under clinician guidance, especially when probiotic use is paired with careful diet quality, sleep, stress management, and bowel habit tracking. But trial language should remain honest: these are adjunct possibilities, not disease-modifying proof.
| Evidence source | Main finding | Limitation you should remember | Clinical interpretation |
|---|---|---|---|
| Seiler et al., Frontiers in Nutrition, 2020 (systematic review) | Some studies showed symptom or biomarker improvement | Small trials, mixed strains, inconsistent outcomes | Potential adjunct, not replacement for gluten-free diet |
| Harnett et al., Nutrients, 2023 (meta-analysis) | Signals for benefit in select clinical parameters | Heterogeneity and low-to-moderate certainty | Reasonable to individualize, not to generalize broadly |
| ACG guideline update, American Journal of Gastroenterology, 2023 | Core management remains strict gluten elimination and follow-up | Limited direct probiotic recommendation strength for celiac treatment | Prioritize evidence-backed fundamentals first |
For people experimenting with probiotics, this practical guide may help distinguish real change from normal day-to-day variability: how to know probiotic supplements are working.
Myth vs fact: probiotics, gluten, and celiac disease
| Myth | Fact | What to do instead |
|---|---|---|
| "All probiotics are automatically gluten-free because they are healthy products." | Some products can carry ingredient or cross-contact uncertainty. | Use a repeatable label and manufacturer screening process. |
| "If a product says gluten-free, I never need to look deeper." | Claims are helpful, but transparency and testing practices still matter. | Check inactive ingredients and quality disclosures. |
| "Higher CFU means better celiac control." | Bigger CFU counts do not guarantee better outcomes for celiac disease. | Select products based on strain evidence and tolerability, not CFU alone. |
| "Probiotics heal celiac damage, so diet precision matters less." | No strong evidence supports replacing strict gluten avoidance with probiotics. | Keep probiotics as optional adjuncts only. |
| "Persistent symptoms always mean I picked the wrong probiotic." | Symptoms may come from gluten exposure, IBS overlap, or other diagnoses. | Escalate to clinician-led workup rather than endless supplement switching. |
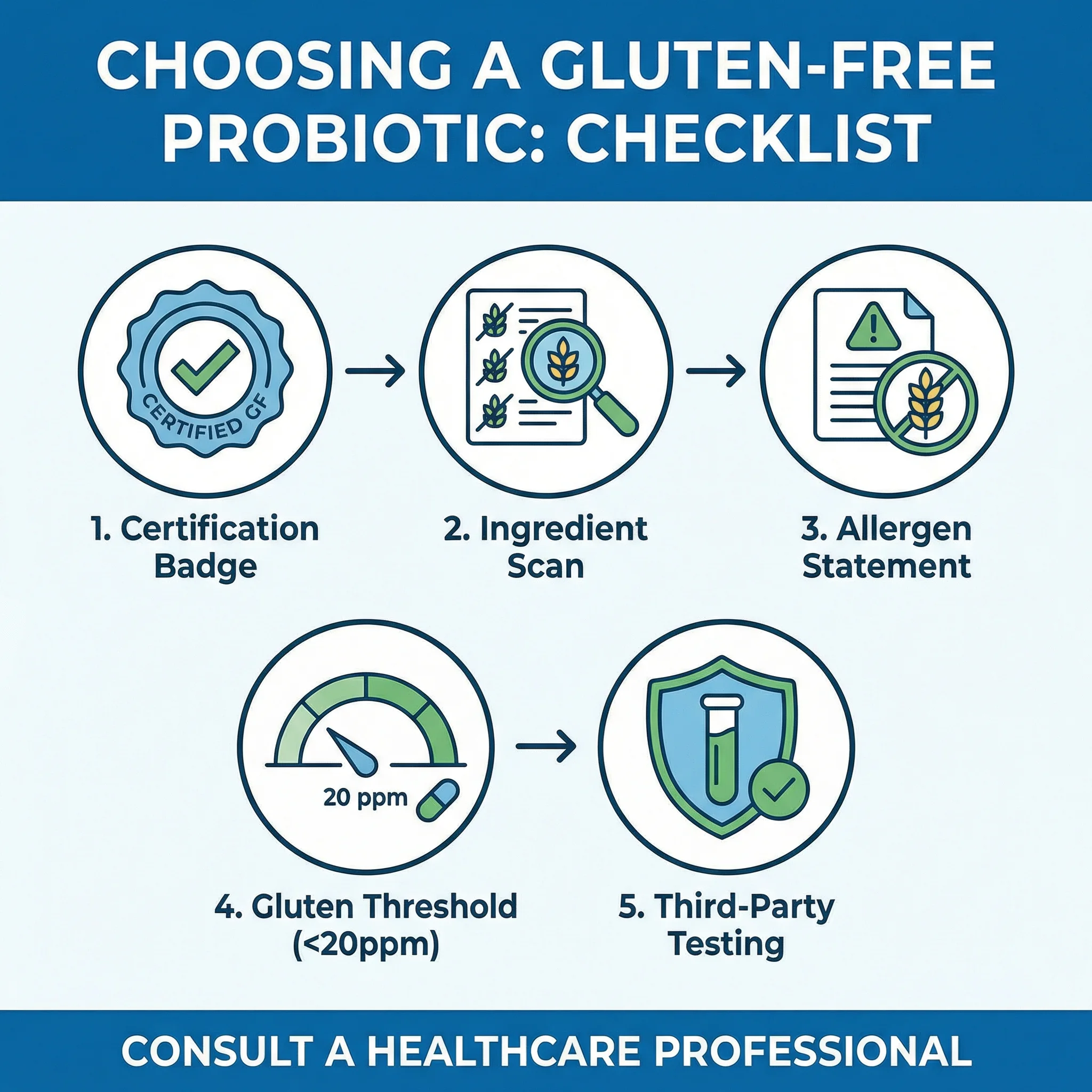
A practical buying framework can lower risk without turning every purchase into a panic loop

The easiest way to reduce decision fatigue is to use the same five-step filter every time. This protects you from impulsive buying and marketing-driven choices, and it keeps your strategy stable across brands and product launches.
- Start with necessity: decide whether you have a clear symptom goal and timeframe for trial.
- Screen for gluten safety first: explicit claim, clear inactive ingredients, and contamination-control language.
- Then screen for evidence fit: strain rationale for your symptom target, not just generic gut claims.
- Limit overlap: avoid stacking multiple new supplements at once.
- Track response objectively for 4 to 8 weeks, then continue, switch, or stop.
Many patients improve their outcomes by simplifying routines before adding supplements. In daily practice, food-first consistency often outperforms supplement complexity. If you are building that base, this food-focused piece is useful: best probiotic foods review.
| Checklist item | Pass signal | Red flag | Decision |
|---|---|---|---|
| Gluten disclosure | Clear gluten-free statement with transparent labeling | No statement or vague allergen language | Reject if unclear |
| Ingredient clarity | Specific excipient names and no ambiguous fillers | Proprietary blend with unclear inactive ingredients | Prefer alternatives |
| Manufacturer transparency | Accessible quality/testing information | No support channel or testing explanation | Downgrade confidence |
| Clinical fit | Defined symptom goal and trial duration | Taking "just in case" without baseline symptoms | Reconsider need |
| Monitoring plan | Simple symptom log and stop criteria | No tracking and frequent random switching | Set structure before starting |
When persistent symptoms mean you should stop self-experimenting and call your clinician
Supplements are easy to buy, which makes them easy to overuse as a substitute for medical reassessment. If your symptoms persist despite strict gluten avoidance and a cautious probiotic trial, the next best step is not another random product. It is targeted clinical evaluation.
- Escalate if you have ongoing weight loss, chronic diarrhea, severe fatigue, or signs of nutrient deficiency.
- Escalate if symptoms worsen after introducing supplements, especially if there is bloating, pain, or bowel instability lasting more than a few weeks.
- Escalate if your diet has become so restrictive that you are under-eating or socially isolated.
A clinician can help separate active gluten exposure from overlapping GI disorders and decide whether additional testing is warranted. This avoids the common cycle where people spend months changing supplements while missing a diagnosis that needs different treatment.
Also remember that "natural" does not always equal "safe for everyone." NIH probiotic safety guidance notes that adverse events are uncommon for many healthy adults but can be clinically significant in higher-risk populations, including those with serious illness or compromised immunity. Context matters.
Frequently Asked Questions
Can I take any probiotic if I have celiac disease?
No. Use a product-level safety screen first. Look for clear gluten-free labeling, transparent inactive ingredients, and manufacturer quality disclosures. Then decide whether probiotic use is clinically necessary for your goals.
Do probiotics heal intestinal damage from celiac disease?
Current evidence does not support probiotics as a replacement for strict gluten elimination in celiac disease. Some studies suggest symptom-level benefits in selected patients, but guideline-level care still centers on lifelong gluten-free diet adherence and follow-up.
Is a higher CFU count always better for celiac symptoms?
Not necessarily. CFU count alone does not determine benefit. Strain selection, product quality, individual tolerance, and symptom target are more important than buying the highest-number label.
How long should I trial a probiotic before deciding it is not helping?
A structured 4 to 8 week trial is usually enough to see whether there is a meaningful symptom trend. If there is no clear benefit, or if symptoms worsen, stop and review with your clinician rather than stacking additional products.
The bottom line is simple: safety screening first, evidence second, and no shortcuts on gluten control
For celiac disease, probiotic decisions should be calm, structured, and evidence-aware. Some products are likely low-risk and reasonable to trial. Others are not worth the uncertainty. The most reliable long-term strategy is to keep the foundation strong: strict gluten-free diet, careful label review, periodic follow-up, and selective supplement use only when goals are clear.
When you treat probiotics as optional tools instead of miracle solutions, you make better decisions and protect what matters most: stable symptom control and intestinal recovery over time.
Selected evidence anchors: Rubio-Tapia et al., American Journal of Gastroenterology, 2023; Seiler et al., Frontiers in Nutrition, 2020; Harnett et al., Nutrients, 2023; Catassi et al., American Journal of Clinical Nutrition, 2007; NIDDK Celiac Disease guidance, 2024; FDA gluten-free labeling and dietary supplement regulatory resources, accessed February 2026.
Medical Disclaimer
This article is for informational and educational purposes only and is not medical advice, diagnosis, or treatment. Always consult a licensed physician or qualified healthcare professional regarding any medical concerns. Never ignore professional medical advice or delay seeking care because of something you read on this site. If you think you have a medical emergency, call 911 immediately.