Crohns Disease
Comprehensive guide to Crohn's disease covering causes, symptoms, diagnosis, and the latest 2025 treatment guidelines including biologics and dietary management.
12 Min Read
Crohn's Disease: The Complete Evidence-Based Guide to Causes, Symptoms, and Modern Treatment
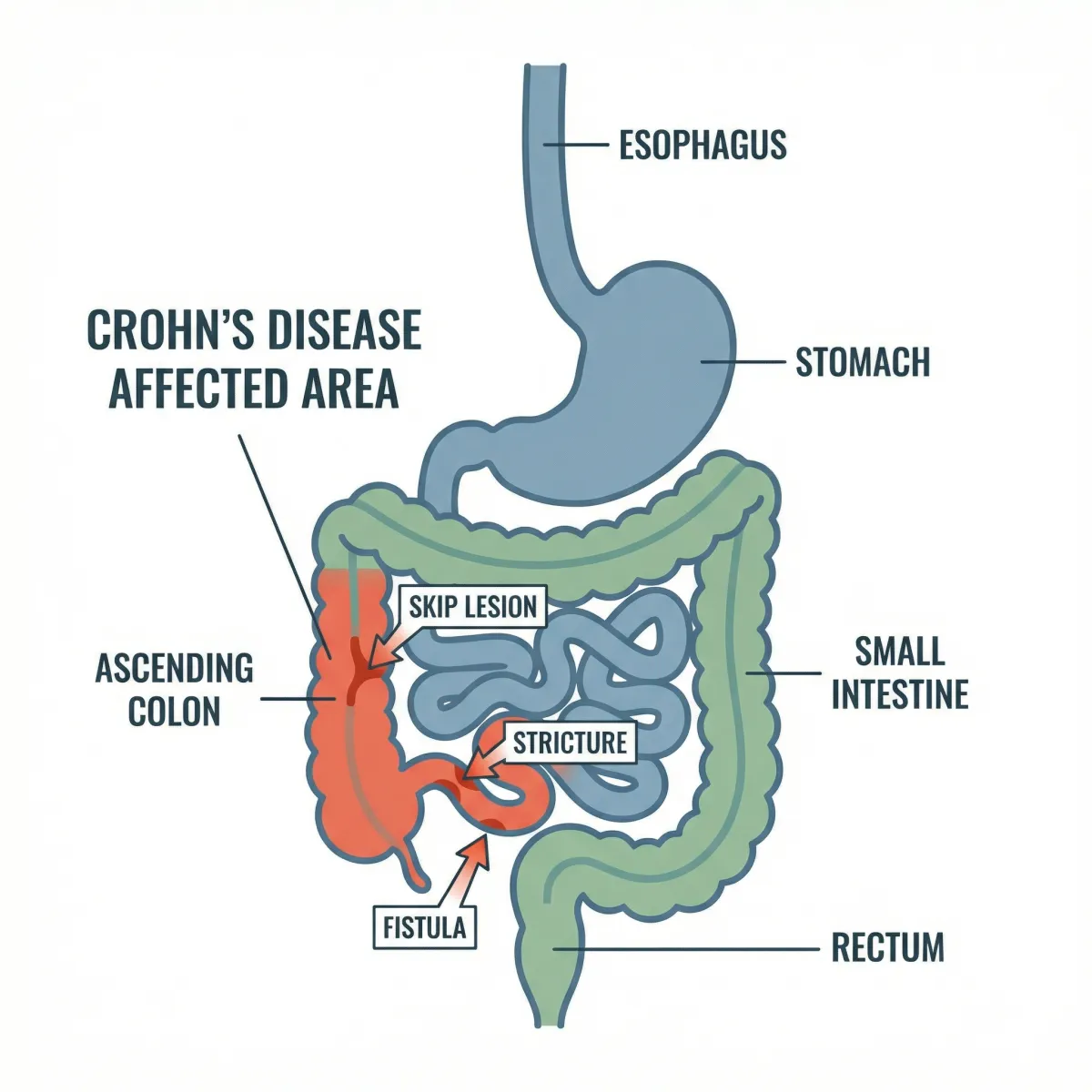
Crohn's disease is a chronic inflammatory bowel disease that can affect any part of the gastrointestinal tract, from the mouth to the anus. Unlike a temporary stomach bug, it involves persistent immune-driven inflammation that damages the intestinal wall in unpredictable cycles of flare-ups and remission. For the millions of people worldwide living with this condition, understanding the latest evidence on its causes, diagnosis, and treatment is not just helpful — it is essential for regaining control over daily life.
Nearly 1 in 100 Americans Now Lives with Inflammatory Bowel Disease
A landmark 2023 study led by the Crohn's & Colitis Foundation estimated that approximately 1.01 million Americans have Crohn's disease, with an overall IBD prevalence approaching 1 in 100 people. Globally, IBD has been accelerating in newly industrialized nations. A comprehensive analysis published in Nature (2025) spanning data from 522 population-based studies across 82 regions showed clear epidemiologic transitions as countries adopt Western lifestyles.
Crohn's disease is one of two main forms of inflammatory bowel disease, the other being ulcerative colitis. While they share some symptoms, their behavior and treatment strategies differ in important ways.
| Feature | Crohn's Disease | Ulcerative Colitis |
|---|---|---|
| Location | Any part of the GI tract (mouth to anus) | Colon and rectum only |
| Inflammation pattern | Patchy, skip lesions | Continuous, starting at rectum |
| Depth of inflammation | Transmural (full wall thickness) | Mucosal (inner lining only) |
| Fistulas | Common | Rare |
| Rectal bleeding | Less common | Very common |
| Granulomas on biopsy | Often present | Absent |
| Smoking effect | Worsens disease | May reduce risk |
According to the CDC, more than 0.7 percent of Americans will be diagnosed with some form of IBD during their lifetime, and prevalence continues to climb. Most people are diagnosed between ages 15 and 35, although the disease can appear at any age, including in children under 10.
What Happens Inside the Body During a Crohn's Flare
In a healthy digestive system, the immune system tolerates the trillions of bacteria living in the gut. In Crohn's disease, that tolerance breaks down. The immune system mounts an aggressive inflammatory response against intestinal bacteria and, in the process, damages the bowel wall itself.
Key fact: Unlike ulcerative colitis, which only affects the inner lining of the colon, Crohn's inflammation penetrates the full thickness of the intestinal wall — a pattern called transmural inflammation. This is why Crohn's is more likely to cause complications like fistulas, strictures, and abscesses.
The inflammation in Crohn's disease tends to appear in patches, with healthy segments of bowel between affected areas. These so-called skip lesions are a hallmark that helps doctors distinguish Crohn's from other bowel conditions. The terminal ileum — the last section of the small intestine before the colon — is the most commonly affected site, though Crohn's can strike anywhere along the digestive tract.
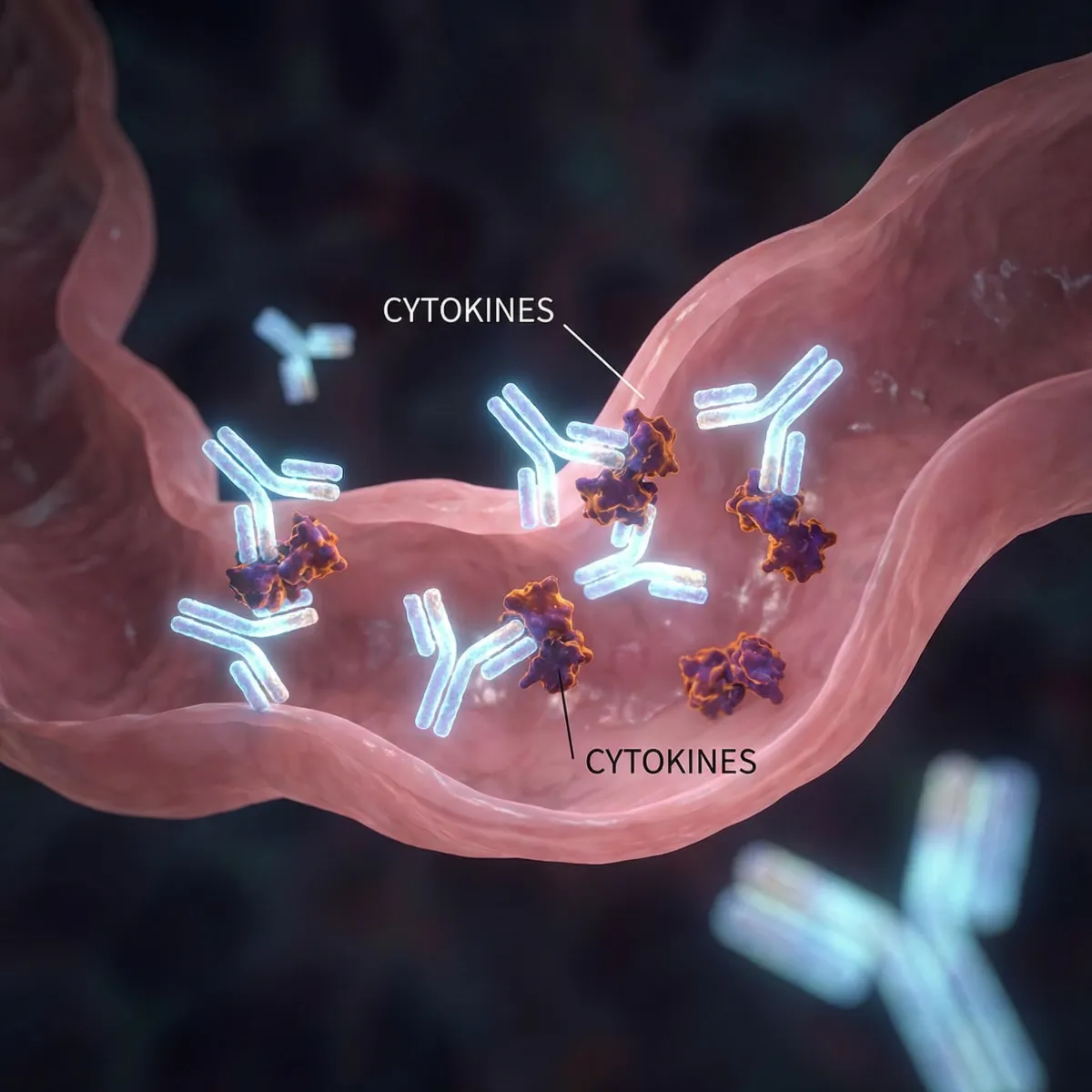
During a flare, the immune cells release cytokines such as tumor necrosis factor-alpha (TNF-α), interleukin-12, and interleukin-23. These inflammatory messengers recruit more immune cells and amplify the damage cycle. Understanding these molecular pathways has led directly to the targeted biologic therapies now used as frontline treatment.
Who Gets Crohn's Disease and Why
No single cause explains Crohn's disease. Current evidence points to a combination of genetic susceptibility, immune dysfunction, environmental triggers, and disruption of the gut microbiome working together to initiate and sustain the disease.
Genetics. Researchers have identified over 200 genetic loci associated with IBD, with roughly 30 showing strong links to Crohn's disease specifically. The NOD2 gene on chromosome 16 was the first discovered in 2001 and remains one of the most significant. Having certain NOD2 variants can increase Crohn's risk by two to four times. Approximately 12 to 15 percent of patients have a first-degree relative with the condition, which is substantially higher than the general population risk.
Immune dysfunction. The colon houses the largest concentration of beneficial bacteria in the body. In genetically susceptible individuals, the immune system misidentifies these commensal organisms as threats. This triggers a sustained inflammatory response that, rather than resolving, becomes self-perpetuating. Research into the role of probiotics in gut health has shown that the composition of the microbiome influences immune regulation and may play a role in IBD susceptibility.
Environmental triggers. Crohn's disease is sometimes described as a disease of industrialization. It is far more prevalent in developed nations with high standards of sanitation. The hygiene hypothesis suggests that reduced childhood exposure to diverse microorganisms impairs the developing immune system's ability to distinguish harmful pathogens from harmless gut bacteria. Other environmental risk factors include:
- Cigarette smoking (doubles the risk of developing Crohn's and worsens disease course)
- Western dietary patterns high in ultra-processed foods and saturated fats
- Prior antibiotic use, especially in childhood
- Urban living environments
- Appendectomy (associated with slightly increased risk for Crohn's, unlike UC)
Recognizing the Warning Signs Beyond Abdominal Pain
Crohn's symptoms can range from mild to debilitating, and they extend well beyond the gut. Recognizing the full spectrum of warning signs helps patients seek diagnosis sooner and avoid complications from untreated disease.
| Symptom Category | Specific Symptoms | Approximate Frequency |
|---|---|---|
| Gastrointestinal | Chronic diarrhea, abdominal pain and cramping, blood in stool | Very common (70-90%) |
| Systemic | Fatigue, fever, unintentional weight loss, reduced appetite | Common (50-70%) |
| Perianal | Fistulas, abscesses, skin tags around the anus | Moderate (30-50%) |
| Musculoskeletal | Joint pain and swelling (peripheral arthritis), lower back pain (sacroiliitis) | Moderate (20-30%) |
| Dermatologic | Erythema nodosum (tender red bumps), pyoderma gangrenosum (deep skin ulcers) | Less common (10-20%) |
| Ocular | Uveitis, episcleritis (eye inflammation and redness) | Less common (5-10%) |
| Hepatobiliary | Primary sclerosing cholangitis, gallstones | Uncommon (5-10%) |
These extraintestinal manifestations affect up to 40 percent of Crohn's patients at some point and can sometimes appear before any digestive symptoms do. Children with Crohn's disease may experience growth delays and delayed puberty because chronic inflammation impairs nutrient absorption during critical developmental periods.
When to see a doctor: Persistent diarrhea lasting more than four weeks, unexplained weight loss, recurrent abdominal pain, blood in the stool, or chronic fatigue warrant prompt medical evaluation — especially if you have a family history of IBD.
Advertisement - Continue Reading Below
How Doctors Diagnose Crohn's Disease Today
There is no single test for Crohn's disease. Diagnosis relies on combining clinical evaluation, laboratory findings, imaging, and endoscopy to build a complete picture.
Colonoscopy with biopsy remains the gold standard. It allows direct visualization of the intestinal lining and collection of tissue samples to confirm the characteristic granulomas and transmural inflammation of Crohn's disease. Small bowel involvement, which colonoscopy cannot always reach, may require upper endoscopy or capsule endoscopy.
Intestinal ultrasound (IUS) is a significant recent advance. The 2025 AGA guidelines now recommend intestinal ultrasound as a non-invasive, radiation-free tool for both initial assessment and ongoing monitoring of disease activity. It provides real-time visualization of bowel wall thickening and inflammation without the preparation required for colonoscopy.
MR enterography uses magnetic resonance imaging to evaluate the small bowel and detect complications such as strictures, fistulas, and abscesses. It is preferred over CT enterography for repeated imaging because it avoids ionizing radiation.
Laboratory tests help support diagnosis and monitor disease activity. These include C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) for systemic inflammation, fecal calprotectin to measure intestinal inflammation specifically, complete blood count to check for anemia, and stool studies to rule out infectious causes of symptoms.
Myth vs. Fact: What Most People Get Wrong About Crohn's
Misconceptions about Crohn's disease persist even among well-meaning friends and family. The Crohn's & Colitis Foundation has identified several persistent myths that can delay treatment or cause unnecessary guilt.
| Myth | Fact |
|---|---|
| Stress causes Crohn's disease | Stress does not cause Crohn's, though it can trigger or worsen flare-ups. The disease has genetic and immunological roots. |
| Diet causes Crohn's disease | No specific food causes Crohn's. However, dietary patterns influence the gut microbiome and can affect disease activity once established. |
| Crohn's and IBS are the same thing | IBS is a functional disorder with no structural damage. Crohn's causes visible inflammation and tissue destruction that can be seen on endoscopy and imaging. |
| Crohn's only affects the digestive tract | Up to 40% of patients develop extraintestinal manifestations in joints, skin, eyes, or liver. |
| Surgery can cure Crohn's disease | Surgery removes damaged bowel segments and treats complications, but the disease can recur in other areas. There is currently no cure. |
| Only older adults get Crohn's disease | Peak diagnosis occurs between ages 15 and 35, and children as young as toddlers can develop the condition. |
| People with Crohn's just need to eat better | While diet helps manage symptoms, Crohn's requires medical treatment to control the underlying immune-driven inflammation. |

Modern Treatment Has Changed the Game
Treatment for Crohn's disease has undergone a fundamental shift. The 2025 guidelines from both the American College of Gastroenterology and the American Gastroenterological Association now recommend starting advanced biologic therapies early in moderate-to-severe disease, rather than the traditional step-up approach that began with less effective medications.
Paradigm shift: The old strategy of starting with aminosalicylates and steroids, then escalating to biologics only after failure, has been replaced. Early use of high-efficacy therapies reduces disease progression, hospitalizations, and the need for surgery.
| Treatment Category | Examples | How They Work |
|---|---|---|
| Anti-TNF biologics | Infliximab, adalimumab, certolizumab pegol | Block tumor necrosis factor-alpha to reduce inflammation |
| IL-12/23 inhibitors | Ustekinumab | Block interleukin-12 and interleukin-23 signaling pathways |
| IL-23p19 inhibitors | Risankizumab, mirikizumab, guselkumab | Selectively block interleukin-23 with improved specificity |
| JAK inhibitors | Upadacitinib | Small molecule that inhibits Janus kinase signaling inside immune cells |
| Anti-integrin therapy | Vedolizumab | Prevents inflammatory cells from migrating into the gut |
| Immunomodulators | Azathioprine, methotrexate | Suppress overall immune activity (often used as combination therapy) |
| Corticosteroids | Budesonide, prednisone | Rapid inflammation control (short-term use only) |
The newer IL-23p19 inhibitors — risankizumab, mirikizumab, and guselkumab — represent a particularly important advance. They target the p19 subunit of interleukin-23 more selectively than ustekinumab, which blocks both IL-12 and IL-23. Clinical trials have shown strong efficacy with favorable safety profiles.
Personalized medicine is also entering clinical practice. The 2025 ACG guidelines recommend assessing genetic markers such as HLADQA1*05 and NUDT15 in select patients to predict responses to specific therapies and reduce the risk of adverse drug reactions. This pharmacogenomic approach helps doctors choose the right medication for each patient from the outset.
Research into natural anti-inflammatory compounds like turmeric and curcumin has generated interest as complementary approaches, though these are not substitutes for proven medical therapies and should be discussed with a gastroenterologist before use.
The Role of Diet in Managing Crohn's Disease
While no diet causes or cures Crohn's disease, nutritional management has become a recognized component of comprehensive care. A 2025 review published in PMC highlights the growing evidence connecting dietary patterns to disease activity and the gut microbiome.
Exclusive enteral nutrition (EEN) — a liquid-only formula diet — is recommended as first-line therapy for children with active Crohn's disease and shows remission rates comparable to corticosteroids without the side effects. The Crohn's Disease Exclusion Diet (CDED) combined with partial enteral nutrition has emerged as a more tolerable alternative with similar efficacy.
Mediterranean dietary patterns appear to have an inverse association with Crohn's disease incidence and may help reduce inflammation in established disease. The DINE-CD clinical trial found that Mediterranean and specific carbohydrate diets showed benefit in patients with mild-to-moderate Crohn's disease, and the 2025 ACG guidelines now recognize dietary therapy as a management option for this patient group.
People living with Crohn's disease should be aware of common nutritional deficiencies that develop from chronic inflammation and malabsorption:
- Iron — from chronic blood loss and impaired absorption
- Vitamin B12 — when the terminal ileum is affected
- Vitamin D — from reduced dietary intake and steroid use
- Calcium — from vitamin D deficiency and lactose intolerance
- Zinc and folate — from generalized malabsorption
Understanding the relationship between gluten sensitivity, celiac disease, and gut inflammation can also be valuable for patients who experience overlapping symptoms or who are managing multiple conditions simultaneously.
Dietary approaches should always be individualized with the guidance of a gastroenterologist and registered dietitian, since food tolerances vary widely among Crohn's patients. There is no universal Crohn's diet — what triggers one person may be well-tolerated by another.
Living with Crohn's: Mental Health and Daily Life
The burden of Crohn's disease extends far beyond physical symptoms. Studies consistently show that people with IBD have significantly higher rates of anxiety and depression compared to the general population — and the relationship runs both ways. Psychological distress can worsen disease activity, and active disease intensifies psychological distress.
The unpredictability of flare-ups creates a unique form of chronic stress. Patients often describe anxiety about sudden bathroom emergencies, fear of eating in social situations, and frustration from the invisible nature of the disease — they may look fine while feeling terrible. This disconnect between appearance and experience can lead to feelings of isolation.
Evidence-based strategies for managing the mental health impact of Crohn's include:
- Cognitive behavioral therapy (CBT) — shown to reduce disease-related anxiety and improve quality of life
- Mindfulness-based stress reduction — helps manage the stress response that can trigger flares
- Regular physical activity — low-impact exercise during remission reduces inflammation markers and improves mood
- Support groups — connecting with others through organizations like the Crohn's & Colitis Foundation
- Integrated care models — gastroenterology teams increasingly include psychologists who specialize in chronic illness
Research into complementary approaches for depression and mental well-being suggests that combining conventional treatment with mind-body practices may offer additional benefit for people managing chronic inflammatory conditions.
Building a strong support network, maintaining open communication with healthcare providers, and supporting overall immune health through nutrition are practical steps that help patients maintain quality of life during remission and cope more effectively during flares.
Frequently Asked Questions
Is Crohn's disease hereditary?
Genetics play a significant role but do not tell the whole story. Having a first-degree relative with Crohn's disease increases your risk to roughly 12 to 15 percent, compared to about 1 percent in the general population. Over 200 genetic loci have been associated with IBD, but environmental factors and the gut microbiome also contribute. Most people with genetic risk factors never develop the disease.
Can Crohn's disease go into permanent remission?
Crohn's disease can enter prolonged remission, sometimes lasting years, with appropriate treatment. However, it is a chronic condition with no known cure, and flares can recur at any time. The goal of modern therapy is to achieve and maintain deep remission — meaning both symptom resolution and mucosal healing confirmed by endoscopy.
What is the difference between Crohn's disease and irritable bowel syndrome?
IBS is a functional disorder that causes symptoms like cramping, bloating, and altered bowel habits but does not damage the intestinal tract. Crohn's disease is an inflammatory condition that causes visible ulceration, structural damage, and complications such as fistulas and strictures. IBS is diagnosed based on symptom patterns, while Crohn's requires endoscopic and histological confirmation.
Do all Crohn's patients eventually need surgery?
No. With the advent of early biologic therapy, the rate of surgery has been declining. However, an estimated 50 to 70 percent of patients may require at least one surgery within 10 to 15 years of diagnosis, typically for complications like strictures, fistulas, or abscesses that do not respond to medical therapy. Surgery is not a cure but can significantly improve quality of life.
Is it safe to get pregnant with Crohn's disease?
Most women with Crohn's disease can have healthy pregnancies, especially when the disease is in remission at conception. Active disease during pregnancy increases the risk of complications, so gastroenterologists recommend achieving remission before conceiving. Many biologic medications are considered safe during pregnancy, though the treatment plan should be reviewed with both a gastroenterologist and obstetrician.
Medical Disclaimer
This article is for informational and educational purposes only and is not medical advice, diagnosis, or treatment. Always consult a licensed physician or qualified healthcare professional regarding any medical concerns. Never ignore professional medical advice or delay seeking care because of something you read on this site. If you think you have a medical emergency, call 911 immediately.